Obstetrics & Gynecology

Overview
Basappa Multi-Specialty Hospital offers trusted and comprehensive care for women through every stage of life. Our Gynaecology & Obstetrics Department provides advanced maternity care, treatment for gynecological conditions, and support for reproductive health in a safe and compassionate environment.
With experienced gynecologists, skilled obstetricians, and modern facilities, we ensure safe deliveries, effective management of high-risk pregnancies, and expert treatment for issues like menstrual disorders, PCOS, infertility, and hormonal problems.
Our dedicated team focuses on personalized care, guiding every woman with comfort, confidence, and medical excellence.
Basappa Multi-Specialty Hospital continues to be a reliable choice for women seeking quality healthcare and specialized maternity services.
Book An Appointment
Symptoms
Obstetrics Diagnosis
- Multiple Pregnancies
- Intrauterine Growth Restriction (IUGR)
- Pregnancy-induced Hypertension
- Gestational Diabetes
- Endocrine Disorders


Gynecology Diagnosis
- Polycystic Ovary Syndrome (PCOS)
- Pelvic Inflammatory Disease (PID)
- Screening for Gynaecological Malignancies
- Perimenopausal and Postmenopausal Symptoms
- Adolescent Gynaecology
Procedures
- Normal Delivery
- Cesarean (C-Section) Delivery
- High-Risk Pregnancy Management
- Ovarian Cyst Removal
- Infertility Evaluation & Treatment
- Colposcopy & Cervical Screening Procedures
- Hysterectomy (Uterus Removal Surgery)
- Laparoscopic Gynecological Surgery
- Fibroid Removal (Myomectomy)
- PCOS & Hormonal Disorder Treatment
- Tubectomy / Family Planning Procedures
Treatments

A hysterectomy is a surgical procedure to remove a woman’s uterus—and sometimes the cervix or surrounding tissues—to treat conditions such as severe fibroids, chronic pelvic pain, heavy menstrual bleeding, endometriosis, uterine prolapse, or cancers of the reproductive organs. Depending on the medical need, it may involve removing only the uterus or additional structures, and can be performed abdominally, vaginally, laparoscopically, or with robot-assisted techniques under general or regional anesthesia. Recovery varies by procedure type, requiring rest, pain management, and a gradual return to normal activities, and the surgery permanently ends menstruation and the ability to become pregnant.

ChatGPT said:
A myomectomy is a surgical procedure to remove uterine fibroids (non-cancerous growths) while preserving the uterus, making it ideal for women who wish to maintain fertility. It is recommended for those experiencing heavy menstrual bleeding, pelvic pain, pressure, frequent urination, or difficulty conceiving due to fibroids. Depending on the size and location of the fibroids, the surgery may be performed through an abdominal incision, with minimally invasive laparoscopic or robotic techniques, or through the vagina using hysteroscopy. Usually done under general anesthesia, myomectomy helps relieve symptoms and improves overall reproductive health and quality of life.

An oophorectomy is a surgical procedure to remove one or both ovaries, performed to treat conditions such as ovarian cysts, endometriosis, pelvic infections, benign or cancerous ovarian tumors, or to reduce cancer risk in high-risk individuals. It may involve removing one ovary (unilateral) or both (bilateral), with the latter causing immediate surgical menopause in premenopausal women. The surgery can be done through an open abdominal incision or using minimally invasive techniques like laparoscopy or robotic surgery, under general anesthesia. Recovery varies depending on the surgical method, and the procedure helps relieve symptoms, treat underlying conditions, and prevent potential health risks.

ChatGPT said:
A salpingectomy is a surgical procedure to remove one or both fallopian tubes and is performed for various medical reasons, including ectopic pregnancy, blocked or damaged tubes, infections, endometriosis, or to reduce the risk of ovarian cancer. It can be done as a unilateral salpingectomy (removal of one tube) or bilateral salpingectomy (removal of both tubes), the latter resulting in permanent infertility. The procedure may be performed through traditional open surgery or minimally invasive laparoscopy, depending on the patient’s condition and urgency of treatment. Typically done under general anesthesia, a salpingectomy offers effective relief from symptoms, prevents complications, and can significantly reduce future cancer risks in high-risk patients.
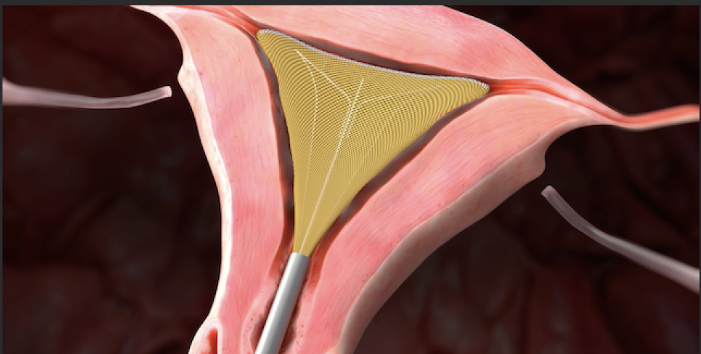
Endometrial ablation is a minimally invasive procedure designed to treat heavy or prolonged menstrual bleeding by removing or destroying the lining of the uterus (endometrium). It is typically recommended for women who have not responded to medication and do not wish to undergo a hysterectomy. The procedure can be performed using various techniques, including thermal, radiofrequency, or freezing methods, and is usually done on an outpatient basis. Endometrial ablation helps reduce menstrual flow, relieve symptoms, and improve quality of life, though it is not intended for women who wish to conceive in the future.
Laparoscopic and hysteroscopic surgeries are minimally invasive procedures used to diagnose and treat a variety of gynecological conditions. Laparoscopy involves small abdominal incisions through which a camera and surgical instruments are inserted to address issues like ovarian cysts, fibroids, endometriosis, and chronic pelvic pain, offering faster recovery and minimal scarring. Hysteroscopy involves inserting a thin camera through the vagina and cervix to examine and treat the uterine cavity, including removal of polyps, fibroids, or adhesions. Both techniques are preferred for their precision, reduced hospital stay, and quicker return to daily activities compared to traditional open surgeries.

Pelvic organ prolapse surgeries are performed to correct the descent of pelvic organs such as the bladder, uterus, or rectum into the vaginal canal, which can cause discomfort, urinary or bowel problems, and a feeling of pressure. Surgical options, including sacrocolpopexy and colporrhaphy, aim to restore the normal position and support of these organs using the patient’s tissue or synthetic mesh. These procedures can be performed through minimally invasive or open techniques, helping improve bladder and bowel function, relieve symptoms, and enhance quality of life while preserving pelvic structure and function.

Tubal ligation and reversal are surgical procedures related to female fertility management. Tubal ligation is a permanent contraception method in which the fallopian tubes are blocked or cut to prevent eggs from reaching the uterus, effectively preventing pregnancy. Tubal reversal is a reconstructive surgery that reconnects the fallopian tubes for women who wish to restore fertility. Both procedures are typically performed using minimally invasive techniques, offering shorter recovery times and reduced surgical risks, with the choice depending on the patient’s reproductive goals and overall health.
High-Risk Pregnancies

Teen Pregnancy (Under 18 Years)
Teen mothers have a higher risk of complications such as preterm birth, low birth weight, anemia, and pregnancy-induced hypertension. Limited prenatal care and nutritional deficiencies may further increase risks.
Advanced Maternal Age (Over 35 Years)
Pregnancy after 35 years is associated with an increased risk of chromosomal abnormalities (such as Down syndrome), miscarriage, gestational diabetes, hypertension, and complications during labor and delivery.

Hypertension (High Blood Pressure)
Can lead to serious complications such as preeclampsia, placental abruption, poor fetal growth, and preterm delivery.
Diabetes (Type 1, Type 2, or Gestational Diabetes)
Increases the risk of large babies (macrosomia), stillbirth, birth defects, and delivery complications.
Heart Disease
May cause serious complications during pregnancy, labor, and delivery due to increased strain on the heart.
Kidney Disease
Can result in poor fetal growth, preeclampsia, and preterm birth.
Autoimmune Disorders (e.g., Lupus, Rheumatoid Arthritis)
Associated with a higher risk of miscarriage, preeclampsia, and fetal growth restriction.
Blood Disorders (e.g., Sickle Cell Anemia, Thalassemia)
Increase the risk of anemia, infections, fetal growth problems, and preterm birth.

Preeclampsia & Eclampsia
Can cause high blood pressure, seizures, organ damage, and fetal distress if not managed promptly.
Gestational Diabetes
May lead to excessive fetal growth, difficult delivery, and neonatal complications.
Placenta Previa
Occurs when the placenta covers the cervix, increasing the risk of severe bleeding and often requiring cesarean delivery.
Placental Abruption
Premature separation of the placenta can cause heavy bleeding and life-threatening fetal distress.
Preterm Labor (Before 37 Weeks)
Increases the risk of breathing problems, infections, and long-term developmental issues in the baby.
Fetal Growth Restriction (IUGR)
The baby does not grow at a normal rate, increasing the risk of complications before and after birth.

Multiple pregnancies carry a higher risk of preterm birth, low birth weight, gestational hypertension, anemia, and delivery complications. Mothers carrying twins or higher-order multiples also require closer monitoring due to increased strain on the body, higher chances of gestational diabetes, preeclampsia, and the need for cesarean delivery. With regular antenatal checkups, specialized care, and timely intervention, many of these risks can be effectively managed to ensure the best possible outcomes for both mother and babies.

Obesity or Underweight
Can increase the risk of gestational diabetes, preeclampsia, birth defects, and delivery complications.
Smoking, Alcohol, or Drug Use
Associated with miscarriage, preterm birth, low birth weight, and congenital abnormalities.
Previous Pregnancy Complications
A history of miscarriage, stillbirth, preterm labor, or cesarean delivery increases the risk in future pregnancies.
Fetal Medicine & Preconception Care

Screening for Chronic Conditions
Conditions such as diabetes, hypertension, thyroid disorders, or heart disease should be identified and well-managed before pregnancy to reduce complications.
Genetic Counseling
Recommended for individuals or couples with a family history of genetic disorders such as sickle cell anemia or cystic fibrosis, helping assess risks and plan appropriately.
Vaccinations
Ensuring immunity against infections like rubella, hepatitis B, and varicella helps prevent serious complications during pregnancy.

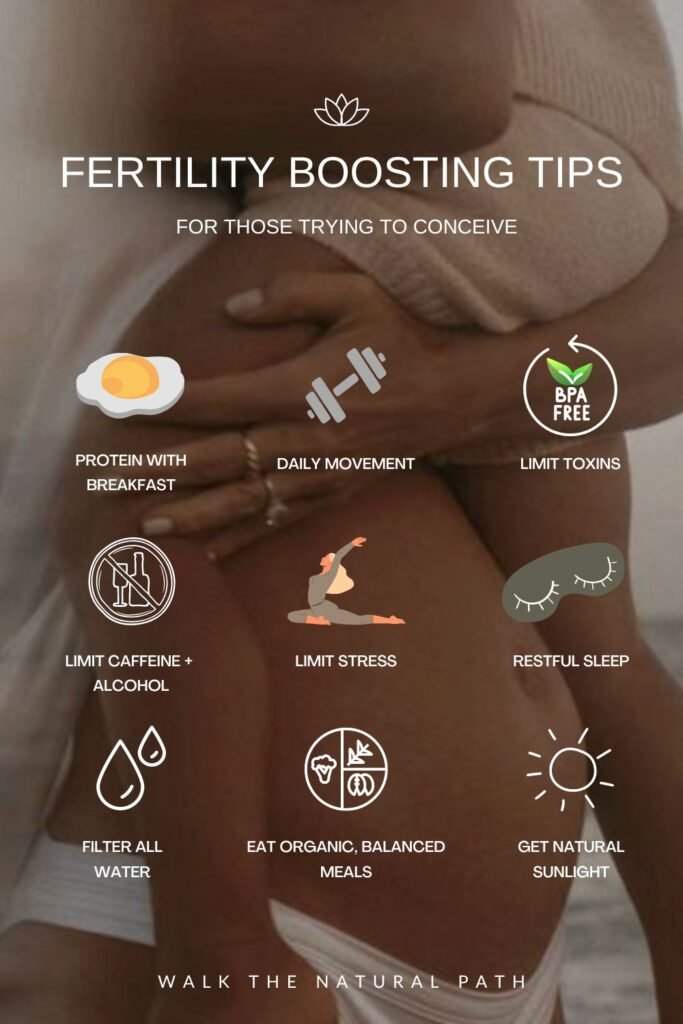
Stop Smoking, Alcohol, and Drug Use
These substances can negatively affect fertility and fetal development and increase the risk of pregnancy complications.
Maintain a Healthy Weight
Being overweight or underweight can interfere with ovulation and increase pregnancy-related risks.
Exercise Regularly
Moderate physical activity helps regulate hormones, improve circulation, and support overall reproductive health.
Reduce Stress
Stress management techniques such as yoga, meditation, relaxation exercises, and counseling can positively impact fertility and overall well-being.

Folic Acid (400–800 mcg daily)
Essential for preventing neural tube defects such as spina bifida.
Balanced Diet
A nutritious diet rich in iron, calcium, vitamin D, protein, and omega-3 fatty acids supports fertility and prepares the body for pregnancy.
Limit Caffeine Intake
Excessive caffeine consumption (more than 200 mg per day) may affect fertility and increase the risk of miscarriage.
Track Menstrual Cycles
Understanding the menstrual cycle helps identify ovulation periods, improving the chances of conception.
Treat Infections
Screening for and treating sexually transmitted infections (STIs) before pregnancy reduces risks to both mother and baby.
Avoid Environmental Hazards
Limiting exposure to harmful chemicals, radiation, toxins, and pollutants at home or in the workplace helps protect reproductive health.
Pregnancy: Stages, Symptoms, and Care
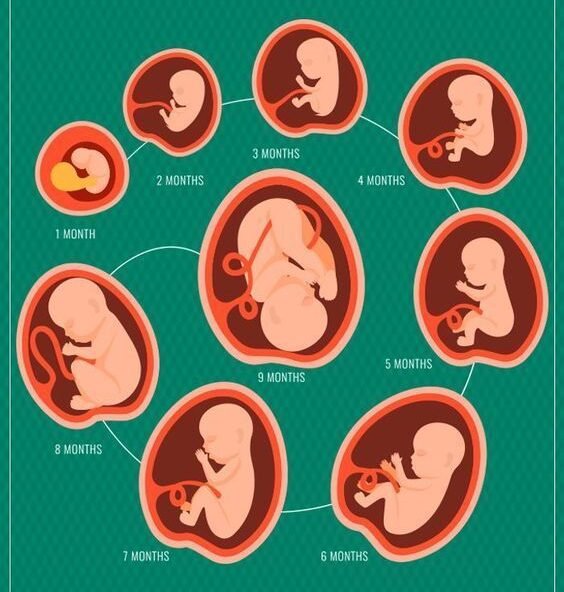
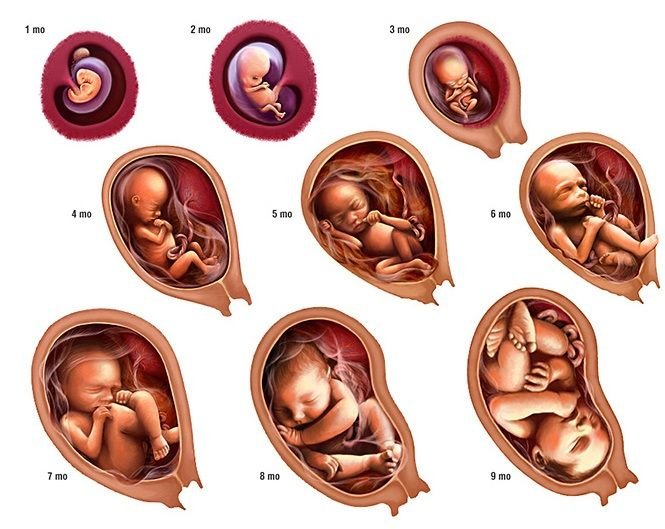
Pregnancy is a remarkable nine-month journey during which a baby grows and develops inside the mother’s womb. This period is divided into three stages, known as trimesters, each lasting about three months. Every trimester brings distinct physical, emotional, and developmental changes for both the mother and the baby. Proper medical care, nutrition, and emotional support throughout each stage are essential to ensure a healthy pregnancy and safe delivery.
Childbirth and Postpartum Recovery
Childbirth occurs in three main stages.
Stage 1: Labor involves the gradual opening (dilation) of the cervix and is divided into three phases. During early labor (0–6 cm dilation), contractions are mild and irregular, this phase may last several hours or even days, and the water may break. Active labor (6–10 cm dilation) is marked by stronger, more frequent contractions with increased pain and discomfort, typically lasting 4–8 hours. The transition phase is the most intense and painful part of labor, with contractions occurring every 2–3 minutes as the cervix completes dilation to 10 cm.
Stage 2: Delivery of the Baby begins once the cervix is fully dilated, the mother starts pushing, and this stage may last from a few minutes to several hours until the baby is delivered.
Stage 3: Delivery of the Placenta follows shortly after birth, during which the placenta is expelled within 5–30 minutes and the uterus continues to contract to prevent excessive bleeding.

The postpartum period is a time of physical and emotional recovery following childbirth. After a vaginal birth, women may experience vaginal bleeding (lochia) for 4–6 weeks, perineal pain if there was a tear or episiotomy, and gradual shrinking of the uterus back to its normal size (involution). Recovery after a cesarean section may involve incision pain and tenderness for several weeks, the need to avoid heavy lifting and strenuous activities, and a longer overall healing period compared to vaginal delivery. Common postpartum symptoms include uterine contractions known as afterpains as the uterus shrinks, breast engorgement when milk production begins, and constipation or hemorrhoids due to hormonal changes and strain during delivery. Emotional well-being is equally important, as some women may experience postpartum depression, characterized by persistent sadness, low mood, or loss of interest, or postpartum anxiety, which includes excessive worry, panic attacks, or sleep disturbances. Early recognition of these symptoms and timely professional support are essential for a healthy recovery.
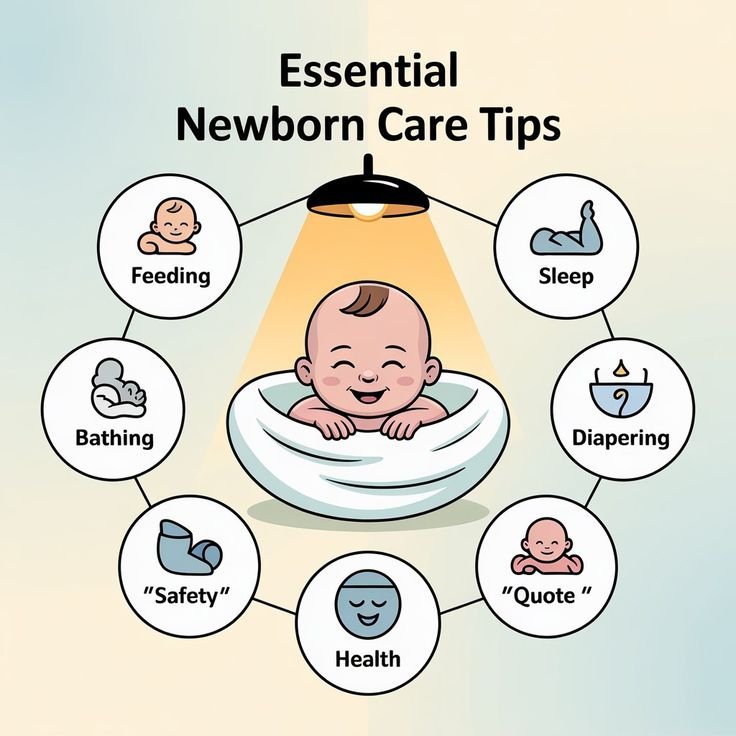
Feeding: Breastfeeding every 2–3 hours or formula feeding every 3–4 hours
Diaper Changes: About 6–8 wet diapers per day
Sleeping: Newborns sleep approximately 16–18 hours a day
Umbilical Cord Care: Keep the area clean and dry; the cord usually falls off within 1–2 weeks
Key Facilities
- State-of-the-art Labour Room with advanced fetal monitoring systems.
- Modern Operation Theatres equipped for normal and high-risk deliveries.
- Experienced Obstetricians & Gynecologists available 24/7.
- Ultrasound & Fetal Imaging Services (2D/3D/4D scans).
- Well-equipped Gynecology Procedure Rooms for minimally invasive surgeries.
- Private & Comfortable Maternity Rooms for mothers and families.

What patients say About Basappa Multi Specialty Hospital Hospitals
Frequently Asked Question
Answers to Your Most Common Questions
What is the right age for a gynecological check-up?
Women should have regular gynecological check-ups starting from their late teens or early twenties, or earlier if they experience symptoms such as irregular periods, pain, or reproductive concerns.
What are the signs of pelvic organ prolapse?
Common symptoms include a feeling of pressure or heaviness in the pelvic area, urinary or bowel difficulties, and visible bulging in the vaginal area.
Is laparoscopic surgery safe?
Yes, laparoscopic surgery is minimally invasive, safe, and associated with quicker recovery, minimal scarring, and reduced hospital stay compared to traditional open surgery.
Can I conceive after endometrial ablation?
Endometrial ablation is not recommended for women who wish to conceive, as it removes the uterine lining, which is essential for pregnancy.
What is the difference between normal delivery and C-section?
Normal delivery is a vaginal birth, while a C-section is a surgical procedure used when vaginal delivery is not safe for the mother or baby.
How can I manage heavy menstrual bleeding?
Treatment depends on the cause and may include medication, hormonal therapy, or minimally invasive procedures like endometrial ablation.
Is tubal ligation reversible?
Tubal ligation is considered a permanent contraceptive method, but tubal reversal surgery can restore fertility in some cases, depending on the patient’s health and tubal condition.
When should I see a gynecologist urgently?
Seek immediate consultation if you experience severe pelvic pain, heavy bleeding, unexplained lumps, abnormal discharge, or symptoms of pregnancy complications.
Your Health Is Our Priority
Schedule your consultation today and experience trusted healthcare with compassion.




